Information on Head Injury
ABI
An acquired brain injury (ABI) is a disruption of normal brain functioning
resulting most often from a sudden traumatic event and can induce
permanent problems ranging from motor control to attention and memory
(Banich, 2004). Although ABI is given great attention from an acute
medical perspective far less consideration is given to the longer
lasting neuropsychological effects (Cassidy et al., 2004). The problems
following an ABI can be crippling to the survivors and their families,
but more knowledge may provide insights that can be used to construct
workable solutions (Temkin, Corrigan, Dikmen, & Machamer, 2009).
TBI
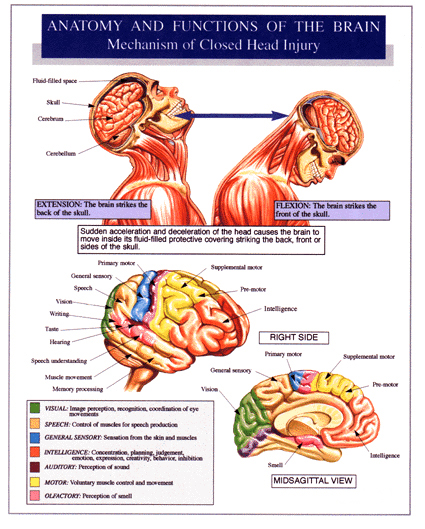
A traumatic brain injury (TBI) is an acquired brain injury resulting
from acceleration-deceleration forces and/or trauma and can result
from open or closed head injuries (Iverson & Lange, 2009). These
injuries represent a significant proportion of trauma admissions
in Canada as well as in the USA. There are an estimated 120, 000
and 1.5 million TBIs sustained annually in both countries respectively
(Canadian Institutes of Health Research, 2006; Mooney, Speed, &
Sheppard, 2005; Iverson & Lange, 2009). TBI is an injury which affects
all ages but particularly adolescents and elderly are at risk (Canadian
Institutes of Health Research, 2006).
TBIs are classified along a spectrum ranging from mild to catastrophic.
The Glasgow Coma Scale and durations of unconsciousness and memory loss following the trauma are most
often used to categorize the injury (Iverson and Lange, 2009). At the lowest end of the traumatic brain injury
scale is where mild is found, the most prevalent classification comprising approximately 70-90% of TBIs (
McKinlay, Grace, Horwood, Fergusson, Ridder, & Macfarlane, 2008).
Problems associated with traumatic brain injury vary depending on the severity but often
include: motor impairments/disorders, deficits in balance and experience of dizziness,
visual impairments, cranial nerve impairments, headaches, sexual dysfunction, fatigue and sleep disturbance,
depression/anxiety disorders, psychotic disorders, personality changes, and lack of awareness
(Ashman, Gordon, Cantor, & Hibbard, 2006; Iverson and Lange, 2009). The appearance and persistence
of these neurological or neuropsychiatric problems follows the gradient of the classification spectrum.
Research has indicated that there are significant alterations in cognitive performance as a result of even mild TBI
(Kwok, Lee, Leung, & Poon, 2008). The prevalence and consequences of mild TBI
creates a clear and obvious need for greater understanding.
MTBI
Mild traumatic brain injury (MTBI) is formally defined by Kay and colleagues
(1993) as a physiological disruption of brain function which has any loss of
consciousness, memory, or alteration in mental state at time of accident. The resulting
effects of MTBI although rarely life threatening are nonetheless health concerns which
may persist for months or longer. They also create a cost for the individual and medical
providers alike (Kraus, Schaffer, Ayers, Stenehjem, Shen, & Afifi, 2005).
|
|
References
Ashman, T. A., Gordon, W. A., Cantor,
J. B., & Hibbard, M. R. (2006). Neurobehavioral consequences
of traumatic brain injury. The Mount Sinai Journal of Medicine,
73(7), 999-1005.
Banich, M. T. (2004). Cognitive
neuroscience and Neuropsychology (2nd Ed.). Boston, MA:
Houghton Mifflin Company.
Canadian Institutes of Health
Research (2006). Head injuries in Canada: A decade of change
(1994 - 1995 to 2003 - 2004)-Analysis in Brief. Canada: Canadian
Institutes of Health Research. Retrieved from www.cihr.ca
June, 2011.
Cassidy, J. D., Carroll, L. J.,
Peloso, P. M., Borg, J., von Holst, H., Holm, L., et al. (2004).
Incidence, risk factors, and prevention of mild traumatic brain
injury: Results of the WHO collaborating centre task force on
mild traumatic brain injury. Journal of rehabilitation Medicine,
43, 28-60.
Iverson, G. L., & Lange, R. T.
(2009). Moderate and severe traumatic brain injury. In M. R.
Schoenberg and J. G. Scott (Eds.), The black book of neuropsychology:
A syndrome based approach. New York: Springer.
Kay, T., Harrington, D. E., Adams,
R., Anderson, T., Berrol, S., Cicerone, K., et al. (1993). Mild
Traumatic Brain Injury Committee, American Congress of Rehabilitation
Medicine, Head Injury Interdisciplinary Special Interest Group.
Defmition of mild traumatic brain injury. Journal of Head
Trauma Rehabilitation,8 (3), 86-87.
Kraus, J., Schaffer, K., Ayers,
K., Stenehjem, J., Shen, H., & Afifi, A. A. (2005). Physical
complaints, medical service use, and social and employment changes
following mild traumatic brain injury: A 6-month longitudinal
study. Journal of Head Trauma Rehabilitation, 20(3), 239-256.
Kwok, F. Y., Lee, T. M. C., Leung,
C. H. S., & Poon, W. S. (2008). Changes of cognitive functioning
following mild traumatic brain injury over a 3-month period.
Brain Injury, 22(10), 740-751.
McKinlay, A., Grace, R. C., Horwood,
L. J., Fergusson, D. M., Ridder, E. M., & Macfarlane, M. R.
(2008). Prevalence of traumatic brain injury among children,
adolescents and young adults: Prospective evidence from a birth
cohort. Brain Injury, 22(2), 175-181.
Mooney, G., Speed, J., & Sheppard,
S. (2005). Factors related to recovery after mild traumatic
brain injury. Brain Injury, 19(12), 975-987.
Temkin, N. R., Corrigan, J. D.,
Dikmen, S. S., & Machamer, J. (2009). Social functioning after
traumatic brain injury. Journal of Head Trauma Rehabilitation,
24(6), 460-467.
|
|